Suicide and Opioid Addiction – Linked Epidemics?
Important note: This article addresses suicide. If you or a loved one is struggling, call the National Suicide Prevention Lifeline at 1-800-273-TALK (8255).
A disproportionately large number of U.S. residents have committed suicide while using an opioid. By definition, we are witnessing an epidemic. Dual diagnosis treatment centers are seeing an increase in patients as they themselves effort to understand the connection between suicide and opioid addiction.
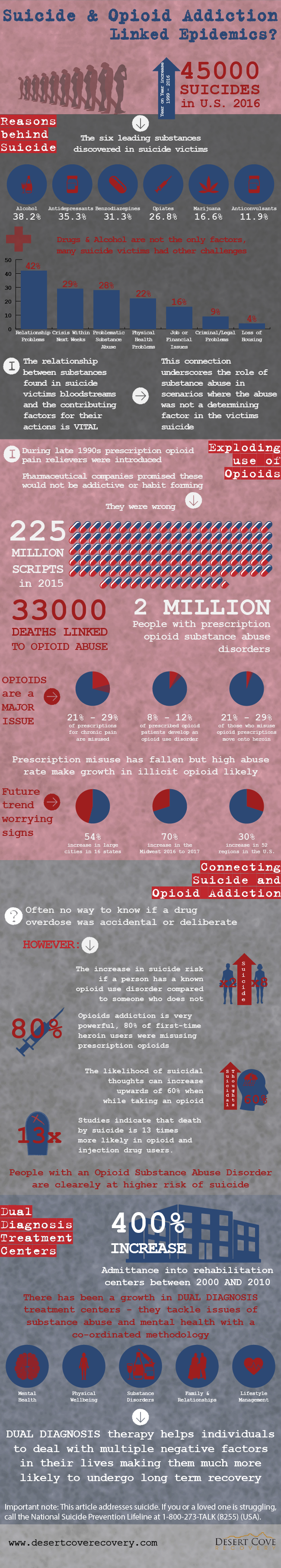
The Centers for Disease Control (CDC) released alarming numbers during the spring of 2018. Their study determined almost 45,000 Americans committed suicide in 2016 alone and discovered an increase of suicide every year since 1999.
The U.S. Surgeon General has advised more Americans use opioids than smoke cigarettes. Considering the U.S. purchases 80% of the world’s opioid medications and prescriptions have increased 300 percent in a nine-year time frame, this makes sense.
Together, it appears opioids and an increasing suicide rate may indeed be linked.
Continued after infographic:
An Increasing Suicide Rate
The relationship between suicide and substance abuse is a complicated one. While suicide is closely correlated with depression, use of either legal or illicit drugs increases the risk substantially. A 2013 study by the CDC revealed which types of substances were found in those who committed suicide. The leading six substances were:
- Alcohol – 38.2%
- Antidepressants – 35.3%
- Benzodiazepines – 31.3%
- Opiates – 26.8%
- Marijuana – 16.6%
- Anticonvulsants – 11.9%
Use of drugs or alcohol is one of the most common risk factors for suicide. However, substance use is only one half of the equation.
In isolation, it would easy to pin a large portion of suicides strictly on substance abuse. But unfortunately, nothing could be further from the truth. In most suicides, substance abuse is the cause or the result of one or more contributing conditions.
The CDC completed a study reviewing the mental reports of both medical examiners and law enforcement officials from 27 states in 2015. They acknowledged there may have been other circumstances involved in any single suicide report, but the result sheds light on the types of problems individuals may have been facing prior to their passing:
- 42% reported relationship problems
- 29% faced a crisis in the past or upcoming two weeks
- 22% had physical health problems
- 16% were confronting job or financial related issues
- 9% tackled criminal legal problems
- 4% lost their housing
The study showed that just over one-quarter (28%) of suicides had reported known problematic substance abuse. Understanding the relationship between the CDC’s statistics of the substances found in the bloodstream with the contributing factors is important. The connection underscores the role substance abuse plays in scenarios where the abuse was not a determining factor in the suicide.
The Exploding Use of Opioids
During the late-1990s, prescription opioid pain relievers were introduced to the general public in mass. It was promised these drugs would not be addictive or habit forming. The pharmaceutical companies were wrong.
The rate of opioid overdose has risen ever since opioids arrived at the corner pharmacy. In 2015, the CDC reported 33,000 deaths directly resulting from an opioid overdose. This includes prescription opioids such as fentanyl, hydrocodone, and methadone, illegally manufactured synthetics, and heroin.
Almost 225 million opioid prescriptions were written in 2015. The CDC study from the same year found approximately 2 million Americans were suffering from prescription opioid substance abuse disorders. The statistics of opioid misuse are staggering:
- 21% – 29% of prescriptions for chronic pain are misused
- 8% – 12% of prescribed opioid patients develop an opioid use disorder
- 4% – 6% of those who misuse opioid prescriptions move onto heroin
Although the sheer number of annual opioid prescriptions has begun to decline, their misuse continues to increase. And as the number of prescriptions decreased, we may begin to see increased heroin and illicit opioid use in the coming years. Consider the following growth in opioid overdoses:
- 54% increase in large cities in 16 states
- 70% increase in the Midwest 2016 to 2017
- 30% increase in 52 surveyed regions in the U.S.
We are in the midst of a public health crisis. The consequences of which are being felt by individuals, families, employers, and entire communities. Finding the link between suicide and opioid addiction will go a long way toward solving this immense problem.
Connecting Suicide and Opioid Addiction
Overdoses, caused by any substance, can often be difficult to evaluate. Was the overdose accidental or were the drugs consumed with a purpose – suicide?
What we do know are the increases in suicide risk associated with an opioid misuse. For men, the suicide risk nearly doubles if they were known to have an opioid use disorder. For women, there has been found to be an eightfold increase in the risk of suicide. Yet in most cases, the final factor causing an overdose is never known.
Opioid addiction is extremely powerful. The fact that 80% of first-time heroin users were misusing prescription opioids first supports this claim. And regardless of how many of the 115 daily opioid overdoses are attributed to suicide, any number larger than zero is too many.
The likelihood of suicidal thoughts can increase upwards of 60% when while taking an opioid. There are studies indicating death by suicide is 13 times more likely in opioid and injection drug users. More evidence that combating opioid addiction’s role in the nation’s suicide crisis cannot be overlooked
The Role of Dual Diagnosis Treatment Centers
Admittance into rehabilitation centers increased 400% in the decade prior to 2010. As more research is conducted and more is learned about the relationship between suicide and substance abuse, the greater positive impact dual diagnosis treatment centers will have on their patients.
Dual diagnosis takes a coordinated approach to mental health disorders and substance abuse. By using a multidisciplinary team of clinicians, patients with co-occurring disorders are much more likely to find long-term success after receiving treatment. Traditional treatment centers are becoming much better at identifying individuals who are suffering from two or more conditions. And if dual diagnosis treatment isn’t available, such facilities are fortunately opening on a regular basis.
After completing programs offered at dual diagnosis treatment centers, individuals will effectively be able to manage both disorders. If you suspect someone you care about may be struggling with suicide and opioid addiction, let them know not only their friends and family are there for them, but specially trained experts. The community supporting those breaking opioid addiction is growing and help is no further than a phone call away.



